EACH MORNING AT 7, Brian Wolf, the fire chief of Racine, Wisconsin, arrives for work in a neglected corner of a building called the City Hall Annex. A stately, Depression-era brick structure on a not-so-stately stretch of parking lots and auto glass shops, the space once held the workshops of a vocational college. Later, it became home to the city’s boxing club—a sign still hangs in the room that held the old ring. More recently, the space was used for storage. “It’s basically a warehouse,” Wolf says. But a few weeks ago, the Annex’s ancillary purpose became an asset. Old items were cleared out, the walls and floors scrubbed down, and rooms stocked with an array of lab tools and boxes of test tubes and pipettes. The result is perhaps the world’s most unassuming Covid-19 testing lab, where Wolf now presides over his fire crew as pipetter-in-chief.
At the start of a shift, the firefighters don gowns, goggles, and medical masks. Then they await a stream of city workers—permit issuers, police officers, lifeguards—who drop by on their way to work. Under careful supervision, each visitor spits into a vial. And for the rest of the day, the firefighters perform the tests, heating up the samples and pipetting liquids from one test tube to the next. “We’re slow at it,” says Wolf. “But like any emergency we respond to, we have to work together. No bickering. No errors. We get it done.” If all goes well, they’ll have results by lunch. They await a simple change of color in the test tubes: Pink is the all-clear; no virus detected. Yellow is evidence of SARS-CoV-2.
The technology used in the tests is called LAMP, or loop-mediated isothermal amplification. It’s similar to PCR—or polymerase chain reaction—the common way of diagnosing Covid-19, in that it looks for genetic traces of the virus. But it’s a stripped-down process, requiring fewer chemical ingredients, test tubes, and equipment. Typically, the method is used to test for diseases like Zika and dengue fever in places that don’t have lab access—or else by farmers who want to find out what pathogen ails their soybeans. But in Racine, it’s part of an experiment: to see how a cheaper, simpler test, if done frequently enough, might hold outbreaks at bay. Instead of sending samples off to a hospital or lab, and potentially waiting days for results, could you test for Covid-19 from the back of a van, or outside a school, or in a city-owned former boxing gym?
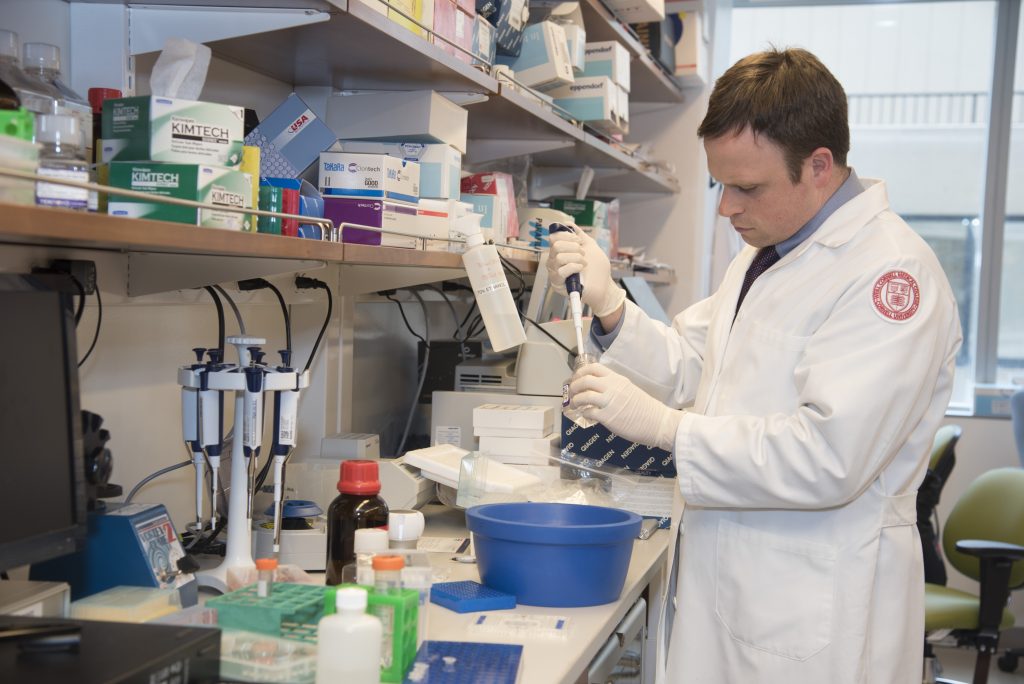 The tests had found their way to the shores of Lake Michigan by way of Chris Mason, a professor at Cornell-Weill Medical School, Racine native, and younger brother of the city’s mayor. Earlier this spring, Mason had published a preprint of his work on LAMP, and then posted it on Facebook and Twitter. It caught his brother’s attention. Their hometown, much like everywhere else, lacked adequate testing for the new virus, and in April, Mason’s brother called, inquiring about his research. The mayor told him that cases were surging, and asked if the test could be put to use.
The tests had found their way to the shores of Lake Michigan by way of Chris Mason, a professor at Cornell-Weill Medical School, Racine native, and younger brother of the city’s mayor. Earlier this spring, Mason had published a preprint of his work on LAMP, and then posted it on Facebook and Twitter. It caught his brother’s attention. Their hometown, much like everywhere else, lacked adequate testing for the new virus, and in April, Mason’s brother called, inquiring about his research. The mayor told him that cases were surging, and asked if the test could be put to use.
The idea behind LAMP testing, according to Mason, is to give every town or city its own capacity to test closer to home. While few places have their own clinically certified labs, “everybody has a fire department,” he says. Because people can have a Covid-19 infection without symptoms, the major barrier to any return to a semblance of normal life—back to school, to work—is the need to test lots of people, regularly, whether they show signs of Covid-19 or not. An estimate from Paul Romer, a Nobel Prize–winning economist at New York University, puts the requirement for doing so safely at more than 35 million tests per day.