Britta Will, PhD ‹ Back To 2020 Winners
2020 Winners
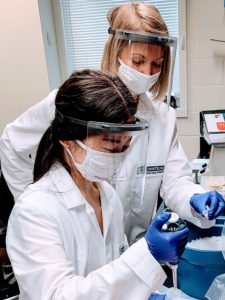
Assistant Professor
Medicine (Oncology)
Albert Einstein College of Medicine / Montefiore Medical Center
Vision
Currently incurable cancers share at least one common feature – therapy-resistant cells which drive disease relapse and progression. In several cancers, these cells are made up by a rare population of functionally and molecularly unique cells, called cancer stem cells. We believe that disabling those molecular pathways cancer stem cells have grown dependent on will allow for the development of curative anti-cancer therapies.
Our research aims at identifying molecular safeguards of cancer stem cells in myelodysplastic syndrome and acute myeloid leukemia – two largely incurable cancers of the blood. We employ clinically relevant and applicable human primary cell-based models as well as rational genetic mouse modeling, along with molecular profiling and functional testing to uncover functionally meaningful networks amenable for therapeutic intervention.
My team and I are passionate for and feel privileged to participating in the search for cancer cures. We hope that our work will ultimately contribute to improving cancer therapy and increasing health span by means of a deeper understanding of fundamental stem cell biology.
Britta Will, PhD is a scientist at the Albert Einstein College of Medicine and a member of the Ruth L. and David S. Gottesman Institute for Stem Cell Biology and Regenerative Medicine, the Institute for Aging Research, and the Stem Cells, Differentiation and Cancer Program at the Albert Einstein Cancer Center. Dr. Will received an M.Sc. from the Technical University of Kaiserslautern, Germany in developmental biology and completed her Ph.D. training in molecular oncology at the Albert Ludwigs University of Freiburg, Germany and Harvard Medical School prior to joining the Albert Einstein College of Medicine for her postdoctoral fellowship in (cancer) stem cell biology. In 2015, Dr. Will was appointed as an assistant professor the departments of Medicine and Cell Biology to pursue her independent research into mechanisms preventing cancerous transformation of adult stem cells. She has made important contributions to our understanding of how healthy blood-forming stem cells sustain their unique functional repertoire and prevent blood cancer formation. Dr. Will has received several awards, including an NIH Career Transition Award, as well as Scholar Awards from the Alexandrine and Alexander L. Sinsheimer Fund, the Gilead Sciences Research Scholars Program in Hematology/Oncology, the Feldstein Medical Foundation and the Leukemia Research Foundation.
Iron homeostasis regulatory pathways in cancer stem cells
Myeloid leukemias are largely incurable cancers of the blood arising from a defective blood stem cell population, termed leukemic stem cells (LSC). Past work, including our own, demonstrated that current therapies for myeloid malignancies fail to eliminate the disease at the stem cell level, providing a path for relapse. We recently uncovered a new role for iron, an essential bioelement required for a vast amount of biological processes, as a functional rheostat in hematopoietic stem cells. We also discovered that therapeutic reduction of intracellular iron leads to a dramatic inhibition of leukemic stem cells while expanding healthy residual stem cells.
“We are immensely grateful for and honored by the generous support of our work by the Pershing Square Sohn Prize which will allow us to break ground on understanding how a novel and likely fundamental molecular pathway hinging on iron sustains cancer stem cells; this knowledge could provide a blueprint for the development of much needed effective cancer stem cell-targeted therapies.”

For our new study, we hypothesize that leukemic stem cells harbor a limited capacity to compensate for changes in the availability of cellular iron. To test our idea, we will use primary human and mouse leukemia models to dissect pathways reestablishing iron homeostasis in cancer stem cells and relying on appropriate iron content; we will also functionally test the consequences of limiting iron availability for LSC maintenance under steady state conditions and during anti-leukemia chemotherapy. Our study may uncover a new biomarker for the detection of LSC, which is an important and unmet clinical need for monitoring therapy efficacy and disease remission. It will also generate key preclinical rationales to therapeutically limit iron availability or inhibit iron homeostasis to render cancerous stem cells more prone to eradication by standard chemotherapy. Lastly, we will provide a new paradigm for iron homeostasis regulatory circuits in the maintenance of other cancer stem cells.
“Innovation is team effort at its best – originating from a conglomerate of passionate, committed and skilled individuals generating and putting an off-the-beaten-path concept to its test; and rooted – particularly in the biomedical space, in a visionary support ecosystem believing in and enabling the realization of a novel idea at a time only a few may back.”