Vinod Balachandran, MD ‹ Back To 2020 Winners
2020 Winners
Assistant Attending/Member
Surgery; Human Oncology and Pathogenesis Program
Memorial Sloan Kettering Cancer Center
Vision
Our goal is to discover new ways to stimulate the immune system to treat cancer through careful study of rare cancer patients with exceptional outcomes. We believe that deep study of these remarkable patients will identify fundamental mechanisms of how the immune system controls cancers, and accelerate the discovery of new effective drugs. We use this approach to study pancreatic cancer, a model deadly cancer that is refractory to all treatments including immunotherapy – and specifically focus on a rare subgroup of pancreatic cancer patients with exceptional long-term survival to discover new immunotherapeutic approaches. Our long-term vision is to use a similar approach of study of biological extremes to usher in the next generation of cancer immunotherapies.
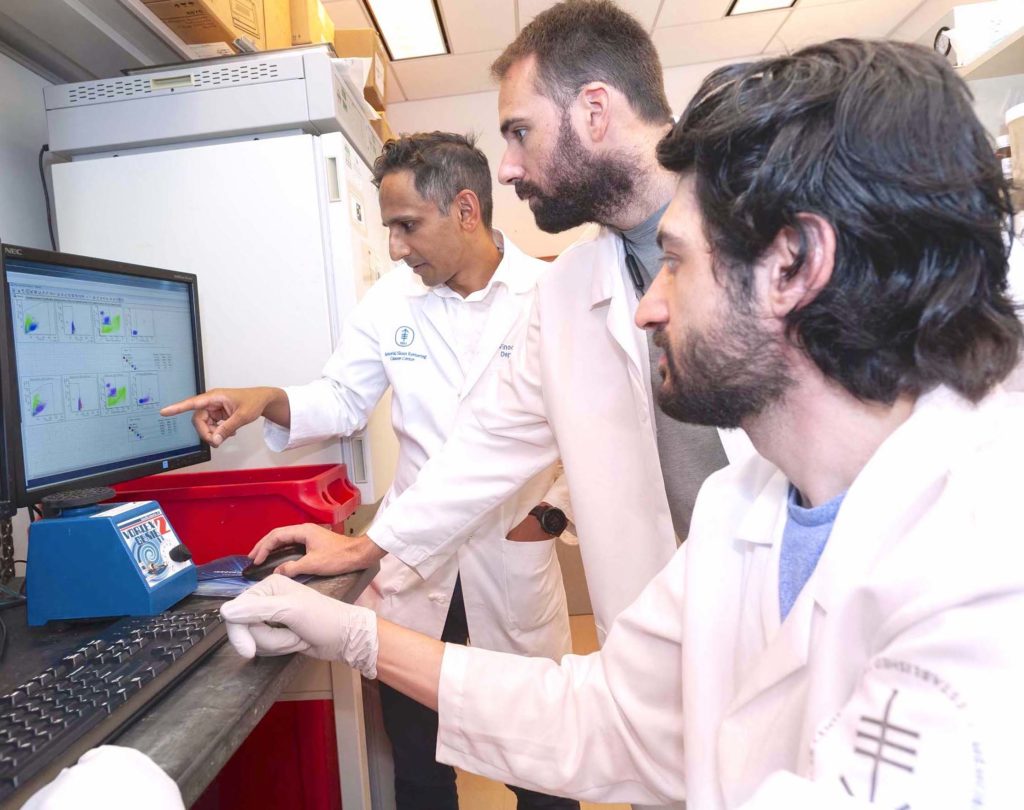
(Featured image photo courtesy of Memorial Sloan Kettering Cancer Center)
Vinod Balachandran, MD is a surgeon-scientist at Memorial Sloan Kettering Cancer Center. Dr. Balachandran completed his undergraduate work in Physics at Cornell University, his MD at the State University of New York at Stony Brook, general surgery residency at Weill Cornell’s NewYork-Presbyterian Hospital, and fellowship training in surgical oncology at Memorial Sloan Kettering Cancer Center. During his surgery training, he pursued postdoctoral work in tumor immunology at the Sloan Kettering Institute, where he identified that kinase inhibitors had partial immune-mediated anti-tumor effects, providing key evidence that kinase inhibitors can be combined with immunotherapy. In 2015, Dr. Balachandran joined Memorial Sloan Kettering Cancer Center as faculty, where he now serves as a principal investigator in the Immuno-Oncology Service of the Human Oncology and Pathogenesis Program (HOPP) and an Assistant Attending Surgeon in the Hepatopancreatobiliary Service in the Department of Surgery. In the clinic, he specializes in the surgical and oncologic care of pancreatic cancer patients and conducts immunotherapy clinical trials. In the laboratory, he leads a basic and translational research program focused on the discovery and application of next-generation cancer immunotherapies for pancreatic cancer. His laboratory studies rare long-term pancreatic cancer survivors and has uncovered key antigens and cells in these patients’ tumors that contribute to their exceptional outcome, findings which are now being translated into therapies for patients. For his work, he has received an American Association of Cancer Research Career Development Award, a Damon Runyon Clinical Investigator Award, a National Cancer Institute Cancer Moonshot Award, and a Stand Up to Cancer Phillip A. Sharp Innovation Award.
Activating Immune Checkpoints on Group 2 Innate Lymphoid Cells for Cancer Immunotherapy
T cells are specialized immune cells that protect the human body from cancer. In the past decade, we have developed revolutionary treatments called immunotherapies that supercharge T cells to kill cancers. Immunotherapies can impressively treat cancer patients more effectively with fewer side-effects even when other therapies have failed. However current immunotherapies are only effective in approximately 20% of patients. Research now shows this is because 80% of tumors have too few T cells to allow immunotherapies to work. Pancreatic cancer is a prime example – patients have a very poor prognosis as standard cancer treatments are ineffective, and, as tumors have few T cells, it is resistant to immunotherapies. Therefore, an effective immunotherapy for pancreatic cancer would be transformative and illuminate new ways to treat many cancers with immunotherapy.
“Pancreatic cancer remains a deadly disease as all current therapies including immunotherapies are ineffective. By studying rare long-term pancreatic cancer survivors who have far outlived their initial prognosis, we have identified that a recently discovered immune cell called group 2 innate lymphoid cells (ILC2s) can control tumors and can be activated using immunotherapies. The Pershing Square Sohn Prize will critically support the study of how these poorly understood cells control tumors, and help catalyze the discovery of new ways to target these cells in the next generation of immunotherapies for pancreatic cancer and other deadly cancers.”

To find new ways to activate T cells in pancreatic cancer, we studied rare long-term pancreatic cancer survivors whose tumors have 12-times as many T cells as other patients’ tumors. We found these tumors also have high numbers of group 2 innate lymphoid cells (ILC2s) – a new cell that stimulates T cells to kill cancers. Using patient tissues and specialized mice with pancreatic cancer, we have discovered a treatment that activates ILC2s, increases T cells in tumors, and allows immunotherapies to control tumors. But the best ways to activate ILC2s in cancer patients are unknown. We will investigate the molecules that control ILC2’s cancer-killing abilities. Our goal is to use this knowledge to effectively activate ILC2s and treat cancer patients with immunotherapy.
“Innovation is to envision the future and make it the present.”