Kyle K. Payne, PhD ‹ Back To 2023 Winners
2023 Winners
Assistant Professor
Department of Medicine
Rutgers Cancer Institute of New Jersey
Vision
Immunotherapy has fundamentally altered the clinical management of cancer, and is potentially curative for some patients with specific malignancies. However, while many patients develop clinically relevant protective immune responses against their tumors, they remain unresponsive to immunotherapeutic interventions – the mechanisms perturbing the clinical benefit in these patients remain unknown. To address this ongoing problem, the overarching vision of our work is to identify novel mechanisms that perturb protective immunity in cancer in order to design a more effective class of cancer immunotherapeutics. We couple our fundamental mechanistic approach with experimental immunotherapeutic methods in unique preclinical xenograft systems to assess potential therapeutic efficacy in the treatment of cancer patients, where we aim to bring the most promising candidates into the clinic. As such, our vision is to fundamentally improve the therapeutic management of cancer by enhancing the efficacy of cancer immunotherapy.
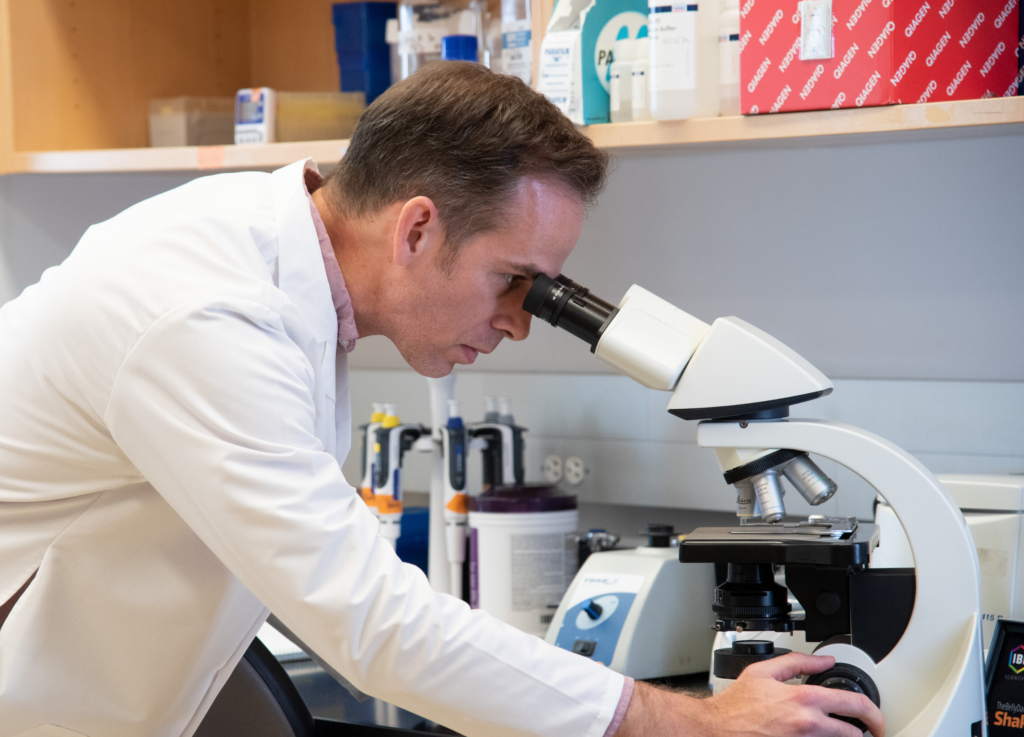
Kyle K. Payne, PhD, is an Assistant Professor in the Department of Medicine at Rutgers University Robert Wood Johnson Medical School, and a resident member of the Rutgers Cancer Institute of New Jersey within the Section of Cancer Immunotherapy. Dr. Payne received a Bachelor’s degree in Biology from Indiana University in 2005, and obtained his Ph.D. in Tumor Immunology from Virginia Commonwealth University in 2015 under the mentorship of Dr. Masoud H. Manjili. He then pursued his postdoctoral training at the Wistar Institute, the University of Pennsylvania, and Moffitt Cancer Center in the laboratory of Dr. Jose R. Conejo-Garcia, where he identified novel mechanisms of immune suppression mediated by checkpoint molecules in the tumor microenvironment. Since joining Rutgers Cancer Institute of New Jersey as a faculty member in 2021, Dr. Payne has turned his attention towards elucidating the intrinsic impact of stress-response signaling pathways within tumor-infiltrating immune cells. His lab currently focuses on understanding how T cell-intrinsic stress-response signaling affects lipid trafficking to regulate protective immunity in the tumor microenvironment. The goal of Dr. Payne’s work is to translate the discoveries in his lab into the clinic in order to produce more effective cancer immunotherapeutics. Dr. Payne is a former American Cancer Society Postdoctoral Fellow; he recently received a V Scholar Grant from the V Foundation for Cancer Research, as well as an Early Career Investigator Grant from the Ovarian Cancer Research Alliance.
Evaluation of Mitochondrial Stress in Orchestrating Lipid Raft Composition in Tumor-Reactive T Cells
 Ovarian carcinoma, the most lethal gynecologic cancer in the western world, kills more than 14,000 American women every year. Current treatments for these women usually include surgery to remove the bulk of the tumor, followed by chemotherapy in an attempt to eradicate any residual tumor cells. While ovarian cancer is usually initially sensitive to chemotherapeutic drugs, the poor 5-year survival rate of these women can generally be attributed to the fact the chemotherapeutic approaches usually fail to eliminate all malignant cells. This drives the development of ovarian cancers that relapse and leads to increased mortality. Therefore, new and more effective approaches are urgently needed in the clinic to complement standard therapeutic approaches to improve the dismal prognosis of ovarian cancer patients.
Ovarian carcinoma, the most lethal gynecologic cancer in the western world, kills more than 14,000 American women every year. Current treatments for these women usually include surgery to remove the bulk of the tumor, followed by chemotherapy in an attempt to eradicate any residual tumor cells. While ovarian cancer is usually initially sensitive to chemotherapeutic drugs, the poor 5-year survival rate of these women can generally be attributed to the fact the chemotherapeutic approaches usually fail to eliminate all malignant cells. This drives the development of ovarian cancers that relapse and leads to increased mortality. Therefore, new and more effective approaches are urgently needed in the clinic to complement standard therapeutic approaches to improve the dismal prognosis of ovarian cancer patients.
“This generous prize will allow us to pursue bold questions; to push beyond what is already known about immune regulation in cancer. With the support of the Pershing Square Sohn Cancer Research Alliance, for the first time we will define a novel system of T cell regulation in cancer. This knowledge will be critical for the design of the next generation of cancer immunotherapeutics.”
 Our immune system has the potential to control cancer and eventually drive the elimination of these malignant cells from the patient’s body. In fact, a specific type of immune cell called a T cell, has a natural ability to recognize and kill cancer cells. Utilizing T cells as an ‘immunotherapy’ against cancer has shown incredibly promising results. This new type of therapy is therefore the most promising anti- cancer strategy since the development of chemotherapy. We are learning, however, that ovarian cancer has developed remarkable strategies to prevent T cell-driven eradication of tumor cells. This proposal therefore aims to uncover and characterize new mechanisms through which ovarian tumors restrain the anti-cancer activity of T cells, and to develop novel approaches to boost T cell activity by targeting these mechanisms.
Our immune system has the potential to control cancer and eventually drive the elimination of these malignant cells from the patient’s body. In fact, a specific type of immune cell called a T cell, has a natural ability to recognize and kill cancer cells. Utilizing T cells as an ‘immunotherapy’ against cancer has shown incredibly promising results. This new type of therapy is therefore the most promising anti- cancer strategy since the development of chemotherapy. We are learning, however, that ovarian cancer has developed remarkable strategies to prevent T cell-driven eradication of tumor cells. This proposal therefore aims to uncover and characterize new mechanisms through which ovarian tumors restrain the anti-cancer activity of T cells, and to develop novel approaches to boost T cell activity by targeting these mechanisms.
“Innovation follows inspiration; the convergence of a desire to know what is not yet known, coupled with an aspiration to apply this knowledge for the benefit of others.”