Xiaolei Su, PhD ‹ Back To 2023 Winners
2023 Winners
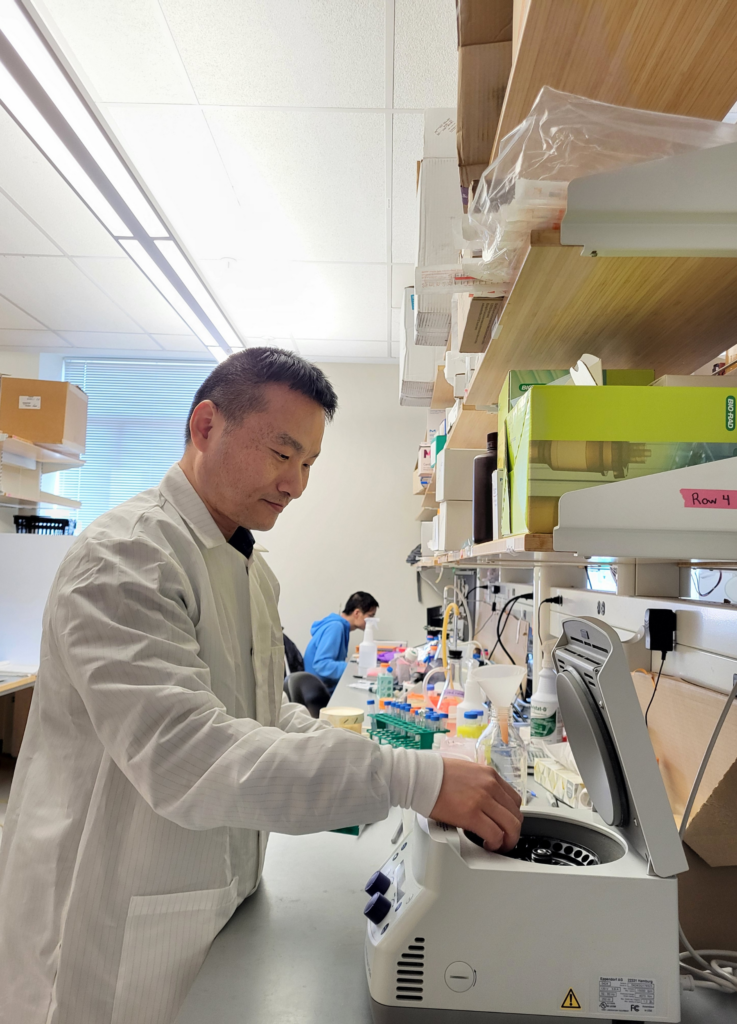
Assistant Professor
Cell Biology
Yale School of Medicine
Vision
The immune system is composed of diverse cell types with varying features. While current cancer immunotherapies, including checkpoint inhibitor and CAR-T, primarily focus on activating T cells to attack cancer cells, the potential of other immune cell types to fight tumors has not been fully utilized. In this project, I aim to repurpose mast cells, a type of long-lived, tissue-resident, and inflammatory immune cells, to target and eliminate solid tumors through designing novel immune receptors tailored to mast cells. This study is expected to create a novel cell therapy that provides more effective and sustained treatment for solid tumors.
Dr. Xiaolei Su earned his bachelor’s degree in science from Peking University and went on to pursue his PhD at Harvard University. Under the mentorship of Dr. David Pellman, he conducted research that uncovered how kinesin-8 motors regulate microtubule dynamics. He then worked as a postdoctoral fellow in Dr. Ron Vale’s Laboratory at the University of California, San Francisco, where he made the discovery that phase separation of membrane-associated proteins promotes T cell activation. Currently, as an assistant professor at Yale University, Dr. Su is leading a passionate and young team dedicated to investigating the mechanisms that mediate immune receptor activation using comprehensive approaches, including protein engineering, biochemical reconstitution, live cell imaging, and mouse models. The knowledge gained from this research is leveraged to develop innovative cell therapies for the treatment of blood, skin, brain, and colorectal cancers. Dr. Su has received numerous awards, including those from the Pershing Square Foundation, Human Frontier Science Program, American Cancer Society, Rally Foundation, Gabrielle’s Angel Foundation, and National Institute of General Medical Sciences.
Engineering mast cells as a novel cell therapy for solid tumors
 Chimeric Antigen Receptor (CAR)-T cell therapies have achieved unprecedented success in treating blood cancers that are resistant to traditional radiation or chemotherapies. However, the efficacy of CAR-T therapy to solid tumors remains limited. Major challenges include poor entering of T cells into tumors, exhaustion and low persistence of T cells under a hostile tumor environment. To tackle these problems, we aim to seek alternative cell weapons that adapt better and live longer in the tumor environment. Mast cells present several advantages over T cells in targeting solid tumors: they reside in tumor tissues and can live up to years. They can repetitively kill target cells without exhaustion. They also release cytokines that can recruit other effector cells to kill cancer.
Chimeric Antigen Receptor (CAR)-T cell therapies have achieved unprecedented success in treating blood cancers that are resistant to traditional radiation or chemotherapies. However, the efficacy of CAR-T therapy to solid tumors remains limited. Major challenges include poor entering of T cells into tumors, exhaustion and low persistence of T cells under a hostile tumor environment. To tackle these problems, we aim to seek alternative cell weapons that adapt better and live longer in the tumor environment. Mast cells present several advantages over T cells in targeting solid tumors: they reside in tumor tissues and can live up to years. They can repetitively kill target cells without exhaustion. They also release cytokines that can recruit other effector cells to kill cancer.
“The Pershing Square Sohn Prize allows me to develop a brand-new immunotherapy, CAR-mast cell therapy, to effectively eradicate solid tumors.”
In this project, we will design CARs that specifically activate mast cells to kill solid tumors, using melanoma and colon cancer as models. Our efforts are expected to lay the scientific foundation for a brand-new cell therapy for solid tumors and this CAR-mast cell therapy will have substantial improved efficacies as compared to the current cell therapies. Following the successful conduct of this project, future work will extend the application of CAR-mast cell therapy to broader types of solid tumors including glioblastoma, lung cancer, and breast cancer.
“My project presents a conceptual innovation in repurposing mast cell, an immune disease-causing cell, for an anti-tumor function.”