Nikhil Joshi, PhD ‹ Back To 2022 Winners
2022 Winners
Assistant Professor
Immunobiology
Yale School of Medicine
Vision
Immunotherapies have curative potential and have fundamentally changed how we treat cancer. Immunotherapy has also changed the way in which we see the immune response to cancer. It is now clear that when many cancer patients enter the clinic, they already have the T cells they need to cure their disease—in their body—and immunotherapy boosts the function of these T cells to eliminate their disease. Yet too many patients do not respond, and why remains unclear. Research in the field has rightfully focused on understanding and fixing the T cells in the tumor, with the goal of improving response rates. However, the tumor microenvironment is damaging to the long-term survival and function of T cells, and we have identified that tumor-infiltrating T cells are replenished from a reservoir located in the tumor-draining lymph node. We believe this lymph node reservoir is protecting T cells and sustaining them long-term, but also that current immunotherapies may not fully utilize these T cells to destroy tumors. Our vision is that by studying these lymph node T cells in engineered animal models, we will be able to uncover mechanisms to better utilize them for therapeutic benefit, which can be translated into immunotherapies that improve response rates for cancer patients.
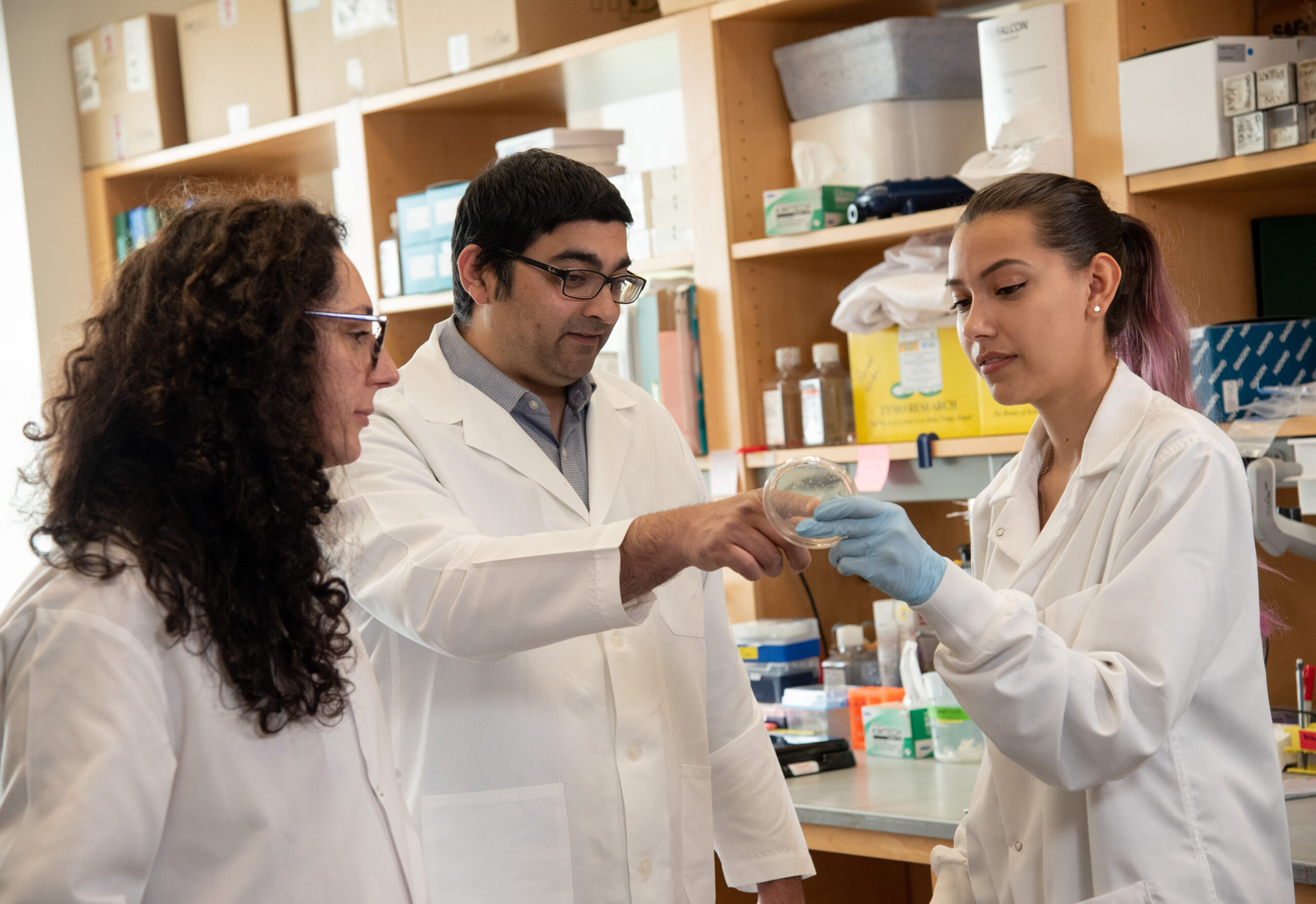
Nikhil Joshi, PhD received his degree in Cell and Molecular Biology from the University of Michigan, Ann Arbor, before obtaining a Science Masters degree from the Johns Hopkins School of Public Health in Molecular Microbiology and Immunology and a PhD in Immunobiology from the Yale School of Medicine. As a PhD student, Dr. Joshi studied the mechanisms by which CD8 T cells decide to become long-lived memory T cells after acute viral and bacterial infections. As a postdoctoral fellow at the Massachusetts Institute of Technology, he started developing engineered animal models that recapitulate human cancer and can be used for the study of cancer immunology. Since returning to Yale as a faculty member in 2016, Dr. Joshi’s laboratory has utilized these models to study the functions of CD8 T cells in developing lung adenocarcinomas, uncovering the central role of the tumor-draining lymph node in maintaining a reservoir of tumor-killing CD8 T cells and in facilitating interactions between these CD8 T cells and other immune cells like B cells and T-follicular helper cells. His lab continues to focus on uncovering basic mechanisms of T cell function with the goal of identifying means to therapeutically drive better T cell responses against established cancers in patients.
Investigating B-T Follicular Helper-CD8 T Cell Interaction in Cancer
 Immunotherapies have shown remarkable effectiveness in curing cancer in patients. They work by revving up T cells that kill tumor cells, but unfortunately, they do not work in most cancer patients. Our objective is to understand why this is and how to fix it. The T cells that immunotherapy will rekindle begin fighting cancer many years before it is detected. Thus, the T cells needed to cure someone’s cancer are in their body when they come in for treatment. However, we have learned that not all T cells respond to immunotherapy.
Immunotherapies have shown remarkable effectiveness in curing cancer in patients. They work by revving up T cells that kill tumor cells, but unfortunately, they do not work in most cancer patients. Our objective is to understand why this is and how to fix it. The T cells that immunotherapy will rekindle begin fighting cancer many years before it is detected. Thus, the T cells needed to cure someone’s cancer are in their body when they come in for treatment. However, we have learned that not all T cells respond to immunotherapy.
“The Pershing Square Sohn Prize will allow my laboratory to engineer complex systems and interrogate how anti-tumor T cells derived from tumor-draining lymph nodes function before and after they enter the tumor. Ultimately, this will lead to a better understanding of what signals drive T cell function and migration, knowledge that can be used to develop the next generation of therapies.”
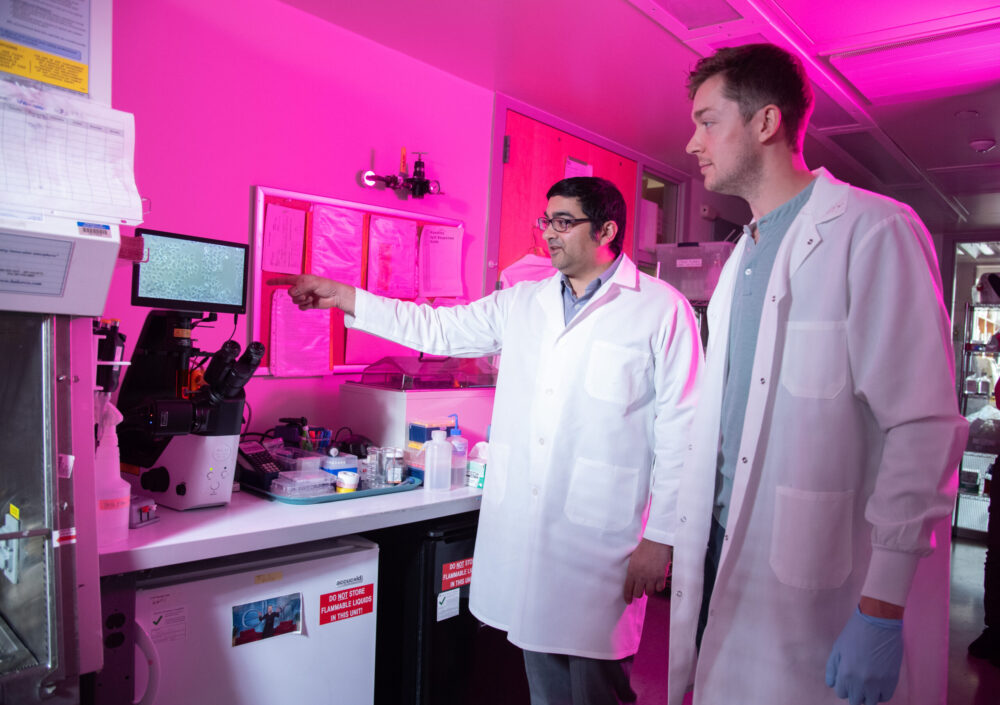 Most studies have focused T cells inside tumor, but we found that, surprisingly, the best T cells for fighting cancer are located outside of the tumor, in nearby glands called lymph nodes. These lymph node T cells are reserves: most lie dormant, but a few travel to the tumor each day to join the fight. We recently showed that T cells can talk with a second immune cell (called a “follicular helper”), which makes them better at fighting when the T cell reaches the tumor. We think that follicular helpers talk to T cells in the lymph node, so we will how they interact, can we make them talk more, and whether other cells are involved. We will use this information to develop therapies that will increase the follicular helpers and drive revved up tumor-killing T cells from the lymph node and into the tumor.
Most studies have focused T cells inside tumor, but we found that, surprisingly, the best T cells for fighting cancer are located outside of the tumor, in nearby glands called lymph nodes. These lymph node T cells are reserves: most lie dormant, but a few travel to the tumor each day to join the fight. We recently showed that T cells can talk with a second immune cell (called a “follicular helper”), which makes them better at fighting when the T cell reaches the tumor. We think that follicular helpers talk to T cells in the lymph node, so we will how they interact, can we make them talk more, and whether other cells are involved. We will use this information to develop therapies that will increase the follicular helpers and drive revved up tumor-killing T cells from the lymph node and into the tumor.
“Therapeutic breakthroughs for patients are built on the right mix of years spent uncovering basic mechanisms, development of enabling technologies, and key insights into disease gained from studies in patients. This requires
a community of investigators who work together and
share findings, with a common goal of improving outcomes
for patients with cancer.”